This article is a brief summary of issues that were identified by the Mobile Dental Clinic and others, as important for the general dental health of residents of RACF, and the ageing in general.
The author is the Principal Dentist of a general dental practice where there was a special interest in addressing the crisis of the poor standards of dental health of the aged population. This was particularly focused at the residents of some local Residential Aged Care Facility (RACF).
Due to lack of funding issues, an established Mobile Dental Clinic (MDC) has unfortunately now been permanently closed, and the assets sold.
Author: By Dr Richard Outridge, B.D.Sc.(Qld), General Practice Dentist
Population changes
It is well documented that the population is ageing (including the current practising dentists). More people are retaining their natural teeth longer, more people are residing in their own homes for longer, the next few years will see a lot of the "baby-boomer" dentists retiring also, and the polypharmacy for patients living longer is getting much more complicated.
Oral and dental health
Many people still think of "dental health" as only related to the teeth, when in fact there is much more to be considered. The gums, all other oral tissues including bone, the swallowing ability, saliva flow and quality, any trauma, eating ability, and just general comfort are some of the less obvious areas considered by dentists when assessing an elderly person’s mouth.
The older generations especially often still only think in terms of (a) ‘Am I in pain now?’, and (b) ‘Can I chew my food?’.
There is much more to consider, and every year we are seeing more research linking dental health to general medical health (and thus to longevity).
Some aspects of the ageing mouth
Figure 1 and Figure 2 (picture below) unfortunately are not uncommon examples of mouths of elderly patients:
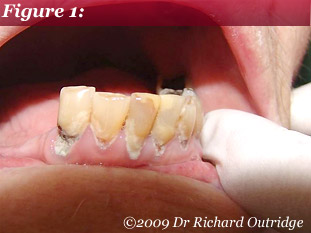 In Figure 1: only the lower front teeth remain and there is no replacement for the back teeth. There is little saliva for lubrication and to aid remineralizing of the teeth. We can see there is much new decay (especially around the necks of the teeth), some of which has been there for some time untreated.
In Figure 1: only the lower front teeth remain and there is no replacement for the back teeth. There is little saliva for lubrication and to aid remineralizing of the teeth. We can see there is much new decay (especially around the necks of the teeth), some of which has been there for some time untreated.
This pattern of decay is typical in an elderly mouth, especially if dry and with a compromised oral hygiene. As a general comment, darker leathery decay is slower spreading compared to very soft yellowy decay which is more aggressive.
We should also not ignore the very real issues of self esteem and appearance that can be adversely affected by such dental conditions. Clarity of speech and an ability to communicate are also important considerations that affect our elderly, and oral health may be a factor to a varying degree in all these issues.
 In Figure 2: we see the upper arch of the same patient. As well as more decay, here we see sharp broken teeth as well, which could cause trauma to the lips, cheeks or tongue.
In Figure 2: we see the upper arch of the same patient. As well as more decay, here we see sharp broken teeth as well, which could cause trauma to the lips, cheeks or tongue.
The skin of the elderly becomes very friable, and the lining of the mouth is no different.
Ulcers caused by sharp edges or damage while brushing can make chewing or swallowing difficult and painful.
But we also note that what saliva is present is frothy. This is not normal.
There are two types of saliva coming from different types of glands in the mouth: They are basically the runny (frothy) type and the stringy type.
Saliva is a whole complex topic in itself - but probably of more interest to oral health professionals!!
Quantity and quality are important however, both to fight decay, and to lubricate tongues, cheeks, and dentures etc.
We need saliva to help dentures stay in place too – for example, two sheets of wet glass are much harder to separate (are more cohesive) than two sheets of dry glass.
The other thing we should note is that while this patient has upper and lower teeth, they will not meet well for chewing.
So the food will not be easily broken down as the first step to digestion and access to nutrition and nutrient absorption by the stomach.
What can you do as a carer?
1. Decay:
- Once decay is present, unfortunately there is little that the lay person can do to repair this. It may need to be treated by a dentist and this can bring a whole raft of new problems such as mobility, availability of services, consent for treatment, treatment costs, apprehension and confusion for the patient, resistance to (safe) access to their mouth by strangers, perhaps discomfort, and sometimes a need to change their daily medication regime to even allow dental treatment (in consultation with their medico et al) – to name a few issues.
- It is MUCH better to try and prevent decay, but again this is a whole topic in itself.
2. Poor saliva flow:
- Today we have access to some very clever research which can provide artificial saliva for rinsing, oral lubricating gels for dry mouths, remineralizing pastes for lowering the risk of decay, a range of tooth pastes with various levels of fluoride to target specific needs, and mouth rinses of various types and efficacy.
- Saliva is essential for lubrication for more comfortable speech and swallowing, for helping fight decay, and is also a small part of the immune system defences.
3. Poor mastication (chewing) of food:
- This can be because of poorly fitting dentures, poorly maintained dentures or natural teeth, a lack of healthy teeth, or poorly occluding (meeting for chewing) natural teeth or dentures. It may be that the patient has reduce muscle control or function too, which may necessitate a change to their denture design (or diet also of course).
- Apart from good hygiene of the dentures and/or natural teeth, there is little that the lay person can do to improve chewing function. Occasionally there is little that even the a dental professional can realistically do to improve chewing, especially if there is a minimal lower ridge supporting a full denture, or an acquired tongue thrust habit, or a non-compliant patient.
- Sometimes the use of proprietary adhesive pastes, pads, or powders may assist denture wearers to gain some stability or retention for chewing. This may also help reduce the effects of a lack of saliva for denture cohesion to the mouth tissues.
- As said, this is an important first step in aiding swallowing and then the absorption of available nutrients from the food. Patients won’t chew if they get pain as a result, but may not be able to communicate that they are in pain, or the origin of their pain...and teeth are often out of sight and out of mind to the inexperienced carer.
- These home carers may also be elderly, and come from a generation which feared anything dental or were (quite reasonably) ignorant of the implications of poor dental health. Education towards oral health is a relatively recent advent.
Conclusion
Oral health is a very complex issue which unfortunately is going to become even more of a problem than it is already. It can be a very expensive issue to address also, and requires a lot of resources applied to the problem. With a better understanding of some of the science of dentistry, there are however some things that carers and the elderly alike can do for themselves to reduce the risks and issues, by prevention and early intervention.
I trust that this short article has highlighted some of the issues or oral health that a lay person can observe and then seek treatment for if appropriate.
By: Dr Richard Outridge, B.D.Sc.(Qld), General Practice Dentist - Date: 29 February 2009